What you should know about Hemodialysis: Life-Saving Treatment for Kidney FailureHemodialysis is an important medical care for people with serious kidney failure, especially people who have been diagnosed with end-stage renal disease (ESRD). In hospital terms, when a patient loses 85-90% of their kidney function and their kidneys no longer adequately filter waste products and extra fluid out of their blood, hemodialysis serves as an artificial replacement.
What is Hemodialysis?
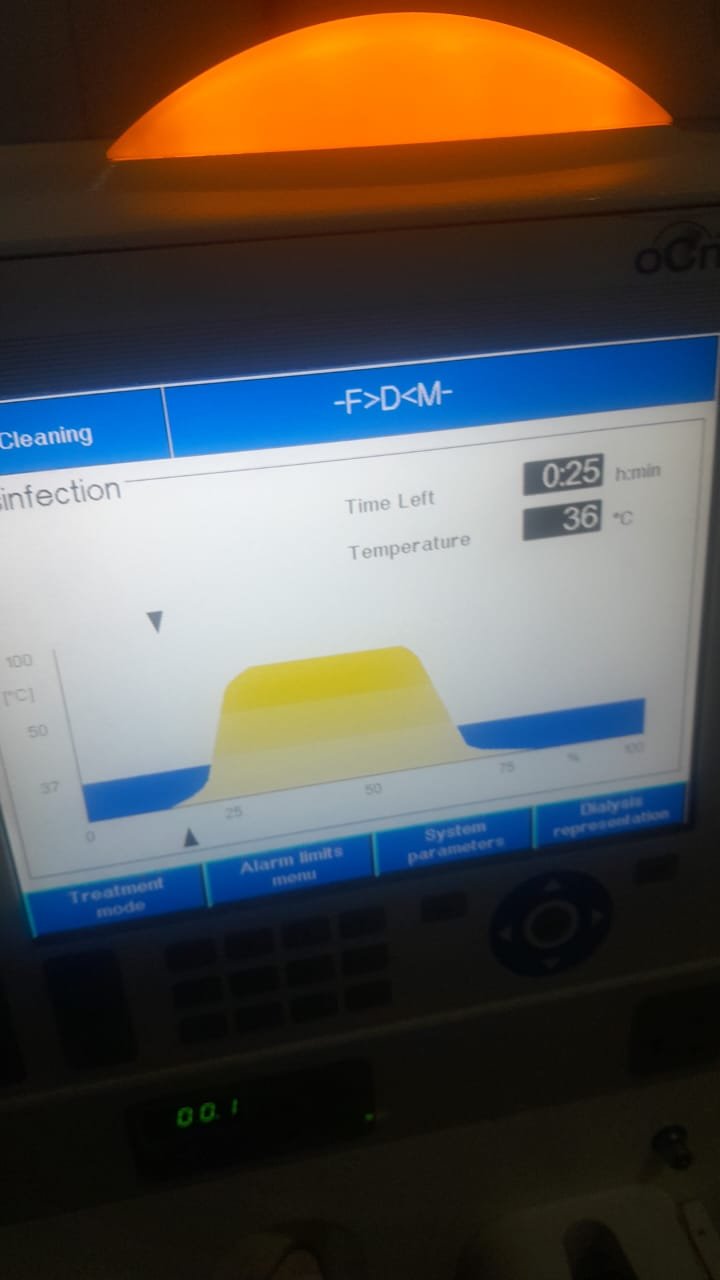
Hemodialysis is a procedure that cleans the blood with a machine and a specific filter called a dialyzer (artificial kidney). It involves taking blood from a patient’s body, filtering it through the dialyzer, and cleaning the blood by removing toxins, waste product, and excess fluid back to the patient.Hemodialysis helps maintain the chemical balance in your body including electrolytes like potassium, sodium, and bicarbonate for normal function.
Dialysis is the primary renal replacement therapy (RRT) for patients with end-stage renal disease (ESRD). With chronic kidney disease (CKD) growing everywhere, the nephrology community must continue to optimize dialysis methods and improve access. This article will review the mechanisms, indications, and recent advancements in dialysis.
Chronic kidney disease affects over 10% of the world’s population, and many of these patients will progress to ESRD which will require dialysis or transplantation. Dialysis serves as an artificial replacement for the excretory function of the kidneys by removing uremic toxins, adjusting electrolyte imbalances, and controlling fluid retention.
When is Hemodialysis Needed
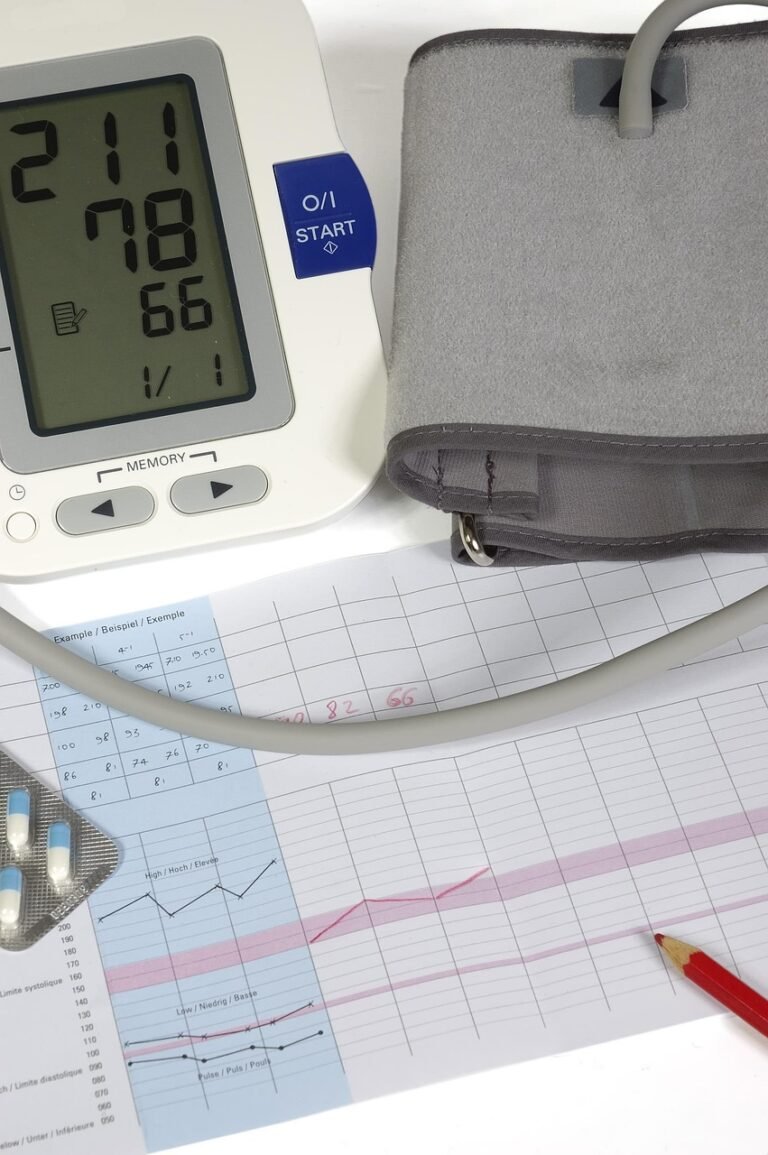
Hemodialysis is usually recommended for patients with:• End-stage kidney disease (ESKD) or chronic kidney disease (CKD) stage 5• Serious complications from acute kidney injury• Persistent symptoms of uremia (buildup of waste products in blood), nausea, fatigue, swelling, confusion, etc. • Dangerous potassium, fluid overload, acid-base status.
What is the process of hemodialysis?
Vascular access: When a person will receive hemodialysis he/she has a vascular access to allow blood to be removed from and returned to his/her body.
There are three main types of vascular access:
- Arteriovenous (AV) fistula – a surgical connection of an artery to a vein
- AV graft – a synthetic tube connecting an artery to a vein
- Central venous catheter – used for temporary access to a large vein, often in an Emergency the Process:The first step is to have blood pumped from the patient’s body into the dialyzer.The dialyzer has a semipermeable membrane that removes waste and fluid, but allows some things to stay in the blood.
The clean blood is then returned to the body.This is usually done 3 times a week over a 3 to 5 hour period, depending on the patient’s needs.
Dialysis Types
Two types of dialysis
- Hemodialysis
Blood is filtered, outside the body, using a machine and a special filter called a dialyzer.
Usually, treatment takes place three times a week for 3–5 hours per session.
Will be either at a dialysis center or at home.
There is external filtration with a dialyzer.
There is a need for a vascular access, or arteriovenous fistula, graft or central venous catheter.
HD can be done in-center or at home. There is also a standard protocol and nocturnal dialysis.
- Peritoneal Dialysis
Utilizes the lining of the abdomen (the peritoneum) to filter the blood inside the body.
A cleansing fluid is instilled into the abdomen through a catheter, absorbs waste, and can be drained.
Typically done daily at home.
PD filters through the peritoneal membrane of the abdomen.
PD includes Continuous Ambulatory Peritoneal Dialysis (CAPD) and Automated Peritoneal Dialysis (APD).
PD may provide more flexibility for lifestyle, but may have an increased risk of peritonitis.
Benefits of Hemodialysis
removes waste and toxins that are not filtered by the Kidney removes symptoms like breathing trouble, swelling, or Dizziness promotes balance of fluids and Electrolytes provides life expectancy and a quality of life for individuals with severe kidney Loss risks and Complications although hemodialysis is life saving, it also has side effects and issues, including:
Low blood pressure while treated muscle Cramping fatigue after treatment, And casualties at the site of access, such as infection, clot formation, Or long-term possible complications, such as anemia or bone Disease living and working with Hemodialysis many people live for years while having dialysis, and they return to work, travel, and enjoy their social life.
However, being on dialysis requires commitment and willingness to change their lifestyle to comply with:Pre-dialysis diet (a diet low sodium, potassium, and phosphorus)
Dietary restrictions on fluid intake between Treatment schedule (must go to treatment, typically 3 times each week)Medical appointments consistently scheduled and Attended alternatives and Forecast kidney replacement therapy options, include:
Peritoneal dialysis (dialysis at home using the peritoneal lining of the abdomen)
Kidney transplantation (if a person is a candidate for kidney transplantation it is usually the best solution over the long term)Although there is no cure for kidney failure, dialysis is a treatment that can extend life and manage symptoms for many patients.
Conclusion:
Hemodialysis is a vital intervention for patients with acute and chronic kidney disease whose kidneys are unable to perform their filtering requirement to survive. Hemodialysis substantially increases quality of life and, with the right attitude to self-care, a person on dialysis can live productive lives.
Overview
Dialysis is a treatment that can take over the function of the kidneys when they become dysfunctional. For the approximately 2 million individuals living with kidney failure, dialysis is a life-sustaining treatment to eliminate excess waste, extra fluids, and toxins from blood.
What Is The Purpose Of Dialysis?
Normal kidneys removes waste products from the blood and helps to maintain equilibrium of body fluids and electrolytes. When your kidneys have damage—particularly from diseases like diabetes, high blood pressure, or chronic kidney disease—they may struggle to perform these processes effectively. If kidney function is below 10-15%, dialysis or kidney transplant is needed to keep you alive.
Complications and Management
Both approaches carry risks; in HD, there are risks of vascular access infection, whereas peritoneal dialysis can result in peritonitis. Managing fluid balance, anemia management, and mineral bone disorder all require ongoing multidisciplinary care.
Recent Developments
We are seeing advances towards the development of wearable dialysis devices and portable machines.
Remote patient monitoring for home dialysis is becoming more prevalent.
Bioartificial kidneys and regenerative therapies are being researched.