Chronic kidney disease (CKD) describes a gradual loss of kidney function over time. As a result of this gradual loss, your kidneys cannot perform some of their important jobs. For example, your kidneys can’t remove wastes and extra fluid from your body. They also help regulate blood pressure.
Table Of Contents
About chronic kidney disease (CKD)
Signs and symptoms
Causes
Complications
Diagnosis
Treatment
About chronic kidney disease (CKD)
Your kidneys do a lot of very important things for your body. Here are just a few ways your kidneys help keep your whole body in balance:1. Remove natural waste products and excess water from your body2. Help make red blood cells3. Help balance your body’s important minerals4. Help control your blood pressure5. Help keep your bones healthy.Chronic kidney disease (CKD) is when the kidneys have become damaged over time (for at least 3 months) and cannot do all of the important kidneys jobs as well as they should. CKD also increases the risk of other health problems like heart disease and stroke. Usually the process of developing CKD is very slow and will have very few symptoms at first over time. For this reason there are 5 stages of CKD to help structure treatment.
Signs and symptoms
Signs and Symptoms most individuals with CKD do not experience symptoms until it is more advanced and/or complications occur. When symptoms do occur, they may include:Foamy urine Urinating (peeing) more often, or less often, than Normal itchy and/or dry skin Feeling tired Nausea Loss of Appetite unexpected weight Loss individuals who have more advanced CKD may notice:Having difficulty Concentrating numbness or swelling in the arms, legs, ankles or Feet achy muscles or Cramping shortness of breath Vomiting Having difficulty sleeping Breath smells like ammonia (that is, urine-like or “fishy” smelling)
Causes
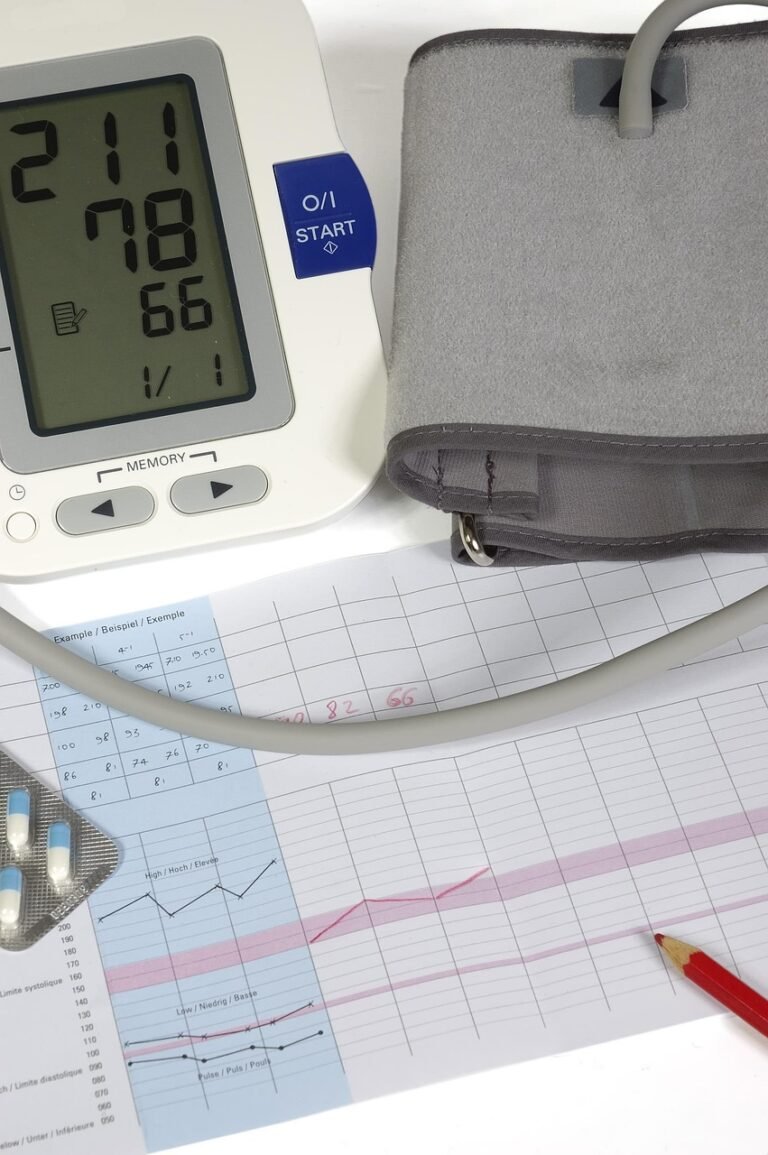
Risk Factors anyone can develop CKD – at any age. However, some people are more at risk than others. The most common risk factors for CKD are:DiabetesHigh blood pressure (hypertension)Heart disease and/or heart failure.ObesityBeing over the age of Family history of CKD or kidney Failure personal history of acute kidney injury (AKI)Smoking and/or tobacco Use for many people, CKD is not caused by just one thing. Instead, it is caused by a combination of many physiological, environmental and social factors. Early detection is important – CKD often begins with few obvious symptoms. Knowing the risk factors can help you assess your level of risk, and if you should be tested for CKD.Other Causes other conditions or circumstances can also cause CKD. For example:Glomerular diseases: glomerulonephritis, IgA nephropathy (IgAN), HIV Nephropathy inherited conditions: polycystic kidney Disease autoimmune conditions: lupus (lupus nephritis)Severe infections: sepsis, hemolytic uremic syndrome (HUS)Others: kidney cancer, kidney stones, frequent untreated and/or long-lasting urinary tract infections (UTIs), hydronephrosis, and birth abnormalities of the kidneys and urinary tract
There are 37 million adults with CKD in the United States – and about 90% are unaware they have it. Take this one minute quiz to find out if you are at high risk for CKD.
Complications
As CKD gets worse, the risk of complications increases. Examples of complications are:Cardiovascular disease (heart disease and/or stroke)High blood Pressure anemia (low levels of red blood cells )Metabolic acidosis (buildup of acid in the blood)Mineral and bone disorder (when minerals of calcium and phosphorus in the blood are not balanced, causing bone and/or heart disease)Hyperkalemia (high levels of potassium in the blood)Kidney Failure some conditions (e.g. cardiovascular disease and high blood pressure), can also lead to, or worsen, CKD
Diagnosis
TestsTesting for CKD is just two simple tests:blood test (termed the estimated glomerular filtration rate [eGFR])urine test (termed the urine albumin-creatinine ratio [uACR])Both tests need to be done in order to assess your kidney function. If your eGFR is less than 60 and/or your uACR is over 30 for three months or longer, it suggests that you may have kidney disease.With respect to the eGFR, it estimates how well your kidneys are removing waste substances from the blood. Your eGFR translates into the body’s ability to filter waste products from the blood. It is calculated from your serum creatinine level, age and sex. It is also possible to calculate your eGFR from your cystatin C level. There are varying definitions of a “normal” eGFR, which differs by age because it declines with age. For these tests, the higher-up will the number, the better! Your eGFR number ultimately determines your stage of CKD.The uACR calculates the amount of two separate substances in your urine – albumin (protein) and creatinine. Healthy kidneys filter the creatinine and most importantly keep albumin in the blood, which means anything we find in your urine for albumin should be negligible or nothing. The calculation of uACR is done by dividing the quantity of urine albumin by the quantity of urine creatinine in order to find the uACR ratio. For this test a lower number is better. Your uACR number is used to test for albuminuria which is a significant risk factor for complications!In certain cases your health professional could order more tests that would help get a better picture of your kidney health. Some examples are kidney biopsy
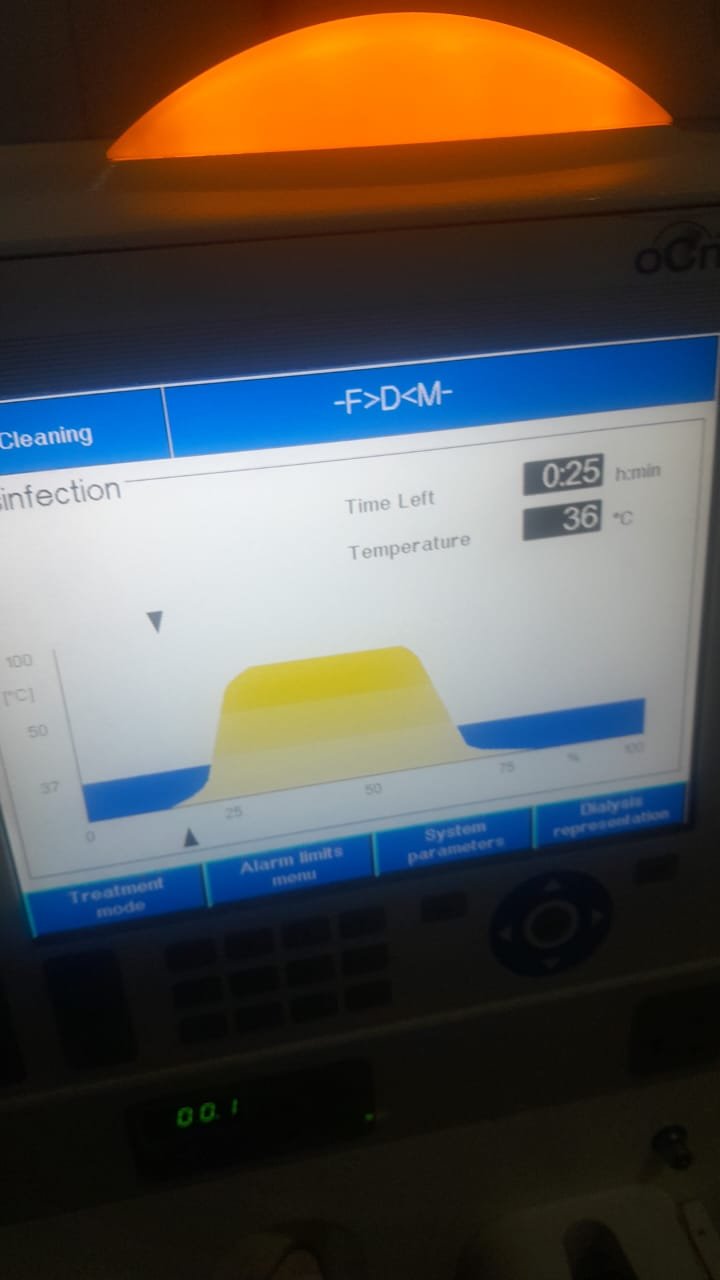
Treatment
Overview management of CKD is focused on four very important goals:Managing the disease(s) or condition(s) that are most likely causing the CKD (for example, your diabetes, high blood pressure, IgA nephropathy)Managing the CKD disease process itself to slow down the CKD disease Progression reducing your risk for cardiovascular disease (having a heart attack or stroke)Treating the complications that you have due to your Specific treatment recommendations depend on your stage of CKD and other health conditions (including CKD complications). Below are general treatment recommendations that apply to most people with CKD. No two people are the same, so talk with your healthcare provider about recommendations based on your individual situation.Medications Your healthcare provider will likely prescribe one or more medicines that will help slow down or stop the progression of your CKD.
These medicines may include an ACE inhibitor/ARB, an SGLT2 inhibitor and/or an nsMRA.Your healthcare provider may also prescribe a statin (cholesterol medicine). Guidelines say to use a statin in persons with CKD with diabetes, cardiovascular disease, or 50 years or older. A statin can be beneficial to lower the risk of a heart attack or stroke even if cholesterol is not high. You may need to take additional medications or supplements to control any CKD complications (if you have any).
Nutrition
It is very important to limit your sodium (salt) intake to less than2300 mg per day (which is about 1 teaspoon of salt from all food and drinks you have each day). This is particularly important if you have high blood pressure. Your health care professional may give you an even lower target based on other health conditions. Limiting sodium means much more than not having a salt shaker at home, it is also limiting sodium foods you eat that are labelled with high sodium levels in their nutrition facts. Even foods that do not taste salty can have a very large amount of sodium when you check their nutrition facts!Depending on your blood tests results your health care professional, or renal dietitian may also suggest you change how much potassium, phosphorus, and/or calcium you may also be consuming from food. Meeting with a dietitian can be especially beneficial if you’re also managing other health conditions such as high blood pressure, diabetes or heart failure – where it’s so much more critical to establish a healthy diet in your life in order to prevent complications. It may feel overwhelming to have to keep track of all the changes, and a dietitian can help.
Tips for changing lifestyles
This is a good time to make healthy lifestyle choices:Stop smoking and/or using tobacco products. Smoking will speed up the kidney disease process and increase your chance of getting kidney failure. Smoking also increases your chance of having other serious health issues, such as high blood pressure, heart disease, cancers, and stroke.Exercise regularly. Remember, start slow – a short walk is a great place to start.Getting enough sleep is important too. Make sure you get enough sleep so that you are well rested.If you are overweight, small changes in eating habits and activity levels can helpIndividuals with CKD should avoid certain pain medications called non-steroidal anti-inflammatory drugs (NSAIDs). NSAIDs can be toxic to your kidneys, particularly at high doses and/or chronic use. Examples of NSAIDs include:ibuprofen (Motrin, Advil)indomethacin (Indocin)naproxen (Aleve, Naprosyn)diclofenac tablets or capsules (Cataflam, Zipsor)celecoxib (Celebrex)meloxicam (Mobic)aspirin (only above 325 mg)Many of these NSAID medications can be obtained over-the-counter (OTC) and may be marketed under a different name or combined with other products (cough & cold products). Sometimes you may have no choice but to use these products based on other health conditions. Always check with your healthcare provider before using any products with those drug names or if the word “NSAID” is written on the label. In general, acetaminophen, also known as Tylenol, is safe for your kidneys – at recommended doses – but check with your healthcare provider first to determine the source of your pain and best way to treat it.