Dialysis is an invaluable treatment for kidney failure patients. It removes waste, excess fluid, and toxins from the blood when the kidneys fail to do so. Like all medical procedures, dialysis can result in some complications. These complications can be minor, short-term complications or possibly more serious long-term complications. When caring for patients, it is important for patients and caregivers to become familiar with and understand these complications so management and prevention can be implemented.
1. Hypotension (Reduced Blood Pressure)
Reduced blood pressure is one of the most frequent complications related to hemodialysis both during and after treatment. This is typically caused by either excessive fluid removal or rapid shifts in fluid balance. Signs and Symptoms: dizziness, weakness, nausea, blurred vision, and faintness.
Prevention: removal of the moderate amount of fluid, limiting large meals prior to dialysis, and modifying the dialysis prescription.
2. Muscle Cramps
Muscle cramps, in particular in the legs, can occur during hemodialysis as result of changes in fluid and electrolytes.
Prevention: an appropriate fluid regimen, stretching exercises, and dialysis duration.
3. Nausea and Vomiting
These may occur due to hypotension or the quick shifting of fluid/electrolytes.
Management involves slowing the rate of dialysis and modifying the volume of fluid removal.
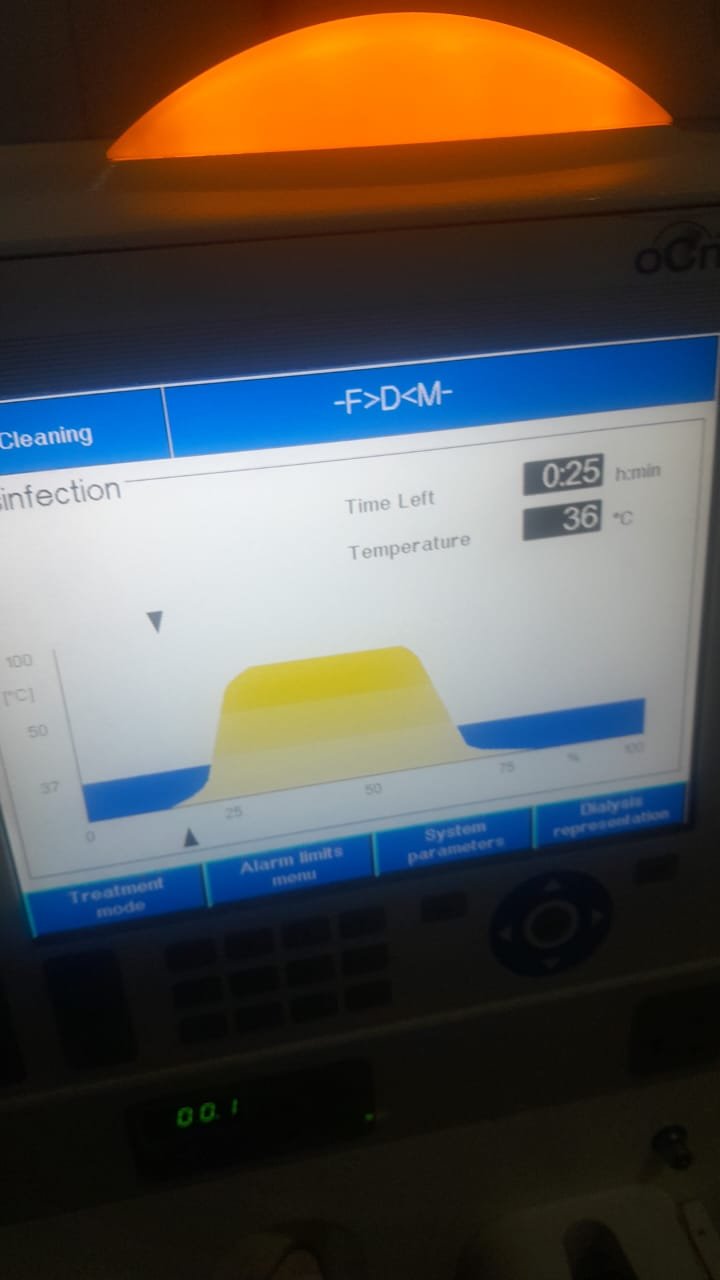
4. Infection
Patients with catheters and fistulas are at risk for infection, which is a serious complication.Infections may be categorized as:
Local infection – at the access or insertion site (may present with redness, pain, swelling, etc.).
Systemic infection (sepsis) – fever, chills, and low blood pressure.
To avoid infection, use strict hand hygiene, appropriate access care, and sterile procedure throughout dialysis.
Problems with Access
Fistulas, grafts or catheters used for access may become clotted, obstructed or infected and negatively affect dialysis efficiency.
Prevention can include monitoring access flow regularly, avoiding pressure on access sites, and seeking medical attention sooner rather than later if there are abnormalities.—
6. Electrolyte Imbalance
Dialysis removes body electrolytes such as potassium, sodium and calcium. A poor balance of electrolytes can cause arrhythmias (irregular heart rhythms), weakness or confusion.
Management includes monitoring lab results closely and modifying the composition of the dialysis fluid.
7. Anemia
Patients receiving dialysis frequently experience anemia because of reduced erythropoietin secretion, and as a result of blood loss associated with dialysis treatments.
Treatment: erythropoietin-stimulating agents (ESAs) and iron replacement.—
8. Bone Disease (Renal Osteodystrophy)
Chronic dialysis patients have an increased risk for calcium-phosphate imbalance and vitamin D deficiency, resulting in weakened/fragile bones.
Prevention: phosphate binders, vitamin D therapy, and a well-managed diet.—
9. Cardiovascular Complications
Patients who are receiving chronic dialysis are at increased risk for cardiovascular disease, hypertension, and fluid overload.Prevention: fluid restriction, healthy blood pressure, and adherence to medication and diet plan.
10. Dialysis Disequilibrium Syndrome
This rare but serious condition follows the rapid removal of toxins from the body, resulting in swelling of the brain.Symptoms include headache, nausea, restlessness, seizures, or a comatose state.
Prevention involves starting dialysis slowly; this is especially important among newer patients.—
11. Itching (Pruritus)
Itching, or pruritus, is a common complaint among patients on dialysis due to elevated phosphorus levels associated with renal failure or dry skin.
Management may include phosphorus control, liberalizing the use of lotions to moisturize the skin, and medications directed for itching.—
12. Psychological Effects
The limitations that are present in the patient’s lifestyles, with or without dialysis, may cause the patient to present with psychological problems, including depression, anxiety, and fatigue.Support may include counseling and patient education, as well as peer support groups.
Conclusion
Dialysis plays a vital role for patients with kidney failure, but can also have complications associated with treatment. Regular assessments, education of patients, maintaining a proper kidney diet, and compliance with medical directives are all factors that can impact risks. A multidisciplinary approach to care helps to create the best possible quality of life for patients on dialysis.